Travelling with Type 1 Diabetes
Preparing for your trip
When travelling with type 1 diabetes, the key is in the planning. With some good preparation ahead of your departure, you’ll be able to handle anything that comes up - just like you do at home.
The following topics covered on this page, which should be used as a general guide only. Speak to your healthcare team ahead of your planned trip, as everyone’s individual needs will vary.
- Packing for travel with type 1 diabetes
- Documents and Travel Insurance
- Airport Security with Omnipod
- Flying with diabetes devices
- Managing meals while flying with type 1 diabetes
- Changing time zones
- Once you’ve arrived and managing type 1 diabetes while you’re away
- Accessing supplies at your destination
- Keeping insulin cool in hot climates
1. Packing for travel with type 1 diabetes
Packing for a short business trip is very different to solo backpacking across the world for two months. Speak to your healthcare team about your specific health needs in relation to the location, duration and type of travel.
Here are some general preparation tips:
Allow enough time
You need time to have conversations with your healthcare providers, and to order your medical supplies. Don’t leave it until the day before!
Write it down
Make a list of all the diabetes equipment you need to pack, using the list below as a starting point. It will also help you keep track of your supplies while you’re away.
More is more!
Your routines on your trip may be very different to everyday life, especially if it’s a vacation, and so you may go through supplies more quickly than normal. Pack extras of everything - more information on that below!
Prepare for the unexpected
There are lots of things that could happen while you’re away, for example an insulin cartridge could break or your supplies could go missing. Hopefully that won’t happen, but packing properly means you’ll be able to adapt to whatever does come your way and get back to enjoying your trip as quickly as possible.
You’ve got this!
There’s no need to be worried. If you live with type 1 diabetes, you’ll already know that things don’t always go to plan, and that having to adapt is part of life with the condition.
How much should you pack?
As a general rule, pack two to three times the amount of supplies you think you will use on your trip1. This will allow for any faults, accidents, delays or very strong waves!
Accidents can happen when you mix diabetes technology with action and adventure but diabetes shouldn’t stop you (or your child) from jumping in the ocean, trying different water sports* or sampling delicious foods.
What should you pack?
Here’s a starter packing list. It will vary between each person, and it’s a good idea to ask your healthcare team for help too.
All diabetes supplies should stay with you in your carry on luggage. Don’t put them into the hold.
Insulet may be able to loan you a back up Personal Diabetes Manager (PDM) or Controller for your trip. Contact our customer care team directly to find out more.
Insulin
Blood Glucose Monitoring
Hypo Treatments
2. Documents and travel insurance for travelling with type 1 diabetes
Diabetes Travel Documents
Diabetes Travel Insurance and the European Health Insurance Card
3. Airport Security with Omnipod
Travelling through airport security with type 1 diabetes can be daunting, but try to remember that airport staff see all sorts of medical equipment everyday, so you don’t need to worry.
These tips should help you feel more prepared and ensure that you pass through smoothly and quickly. You shouldn’t put your diabetes supplies in the hold, so you will need to carry everything with you through airport security.
- Use a separate plastic bag for your liquid medical supplies like insulin; you do not have to put them in the clear bag you use for toiletries and other liquids.
- Check with the airline that you are flying with for their specific requirements. You may even be given additional baggage allowance for your medical supplies3.
- You are allowed to carry all of your diabetes supplies through airport security, including needles and syringes.
- Diabetes supplies and devices may need to be checked, but this is normal. Have your medical letter with you and allow for a little extra time.
- Tell staff that you are wearing a medical device before the screening begins. You should not have to remove your devices.
The medical letter should detail your medication (including your liquids), as well as any supplies you need to carry such as needles, and your Omnipod.
Remember, people with all types of medical conditions pass through airport security every day. There is nothing to worry about.
Can Omnipod go through airport security scanners?
Omnipod Pods, PDMs and Controllers can safely pass through airport x-ray machines.
The Pod, PDM and Controller can tolerate common electromagnetic and electrostatic fields, including airport security and mobile phones.
Pods are safe to be worn through airport scanners.
For glucose sensors, refer to the individual manufacturer’s guidance, as they may not be able to go through x-ray scanners.
If you’d rather not go through the full-body scanner wearing your devices, you can request a manual check, also known as a pat down. Your devices, and your hands, may be tested separately (swabbed)4 - but this is quick and there is nothing to worry about.
4. Flying with diabetes devices
You should keep all of your diabetes supplies with you in the cabin. Never put insulin in the hold when flying as it could freeze, which will damage it1,3. Hold luggage can also get lost.
The Bluetooth® setting remains enabled in the Omnipod PDM/Controller’s aeroplane mode so you can communicate with your Pod.
Your glucose sensor will still work if your phone is in aeroplane mode, and you can use it during the flight - just remember to keep your Bluetooth® on.
Flying with Omnipod
Omnipod is safe to use at atmospheric pressures typically found in aeroplane cabins during a flight.
However, the atmospheric pressure in the cabin can change during flight, and which may affect the pod’s insulin delivery.
Rapid changes in altitude and gravity, such as those typically found during flight take-off and landing, can affect insulin delivery, leading to possible hypoglycaemia or injury. If needed, follow your healthcare provider's treatment instructions.
Always check your blood glucose levels frequently when flying.
5. Managing meals while flying with type 1 diabetes
Pack plenty of snacks and hypo treatments. You need to account for the journey itself and for any travel delays, but also bear in mind that shops may not be immediately accessible at your destination - especially if you are arriving late at night.
If you are unsure about taking liquids through airport security, stick to foods like glucose tablets, sweets and cereal bars which can all be taken through airport security.
It can be hard to calculate carbohydrate amounts for aeroplane meals. If you wait for the food to arrive, you can look at it and judge the amount of insulin you need.
If you want to, you can explain to the cabin crew at the start of the flight that you have type 1 diabetes, and they may be able to tell you roughly what time the meals will be served, and serve your food first. You can bring your own (non-liquid) food on the flight if you prefer.
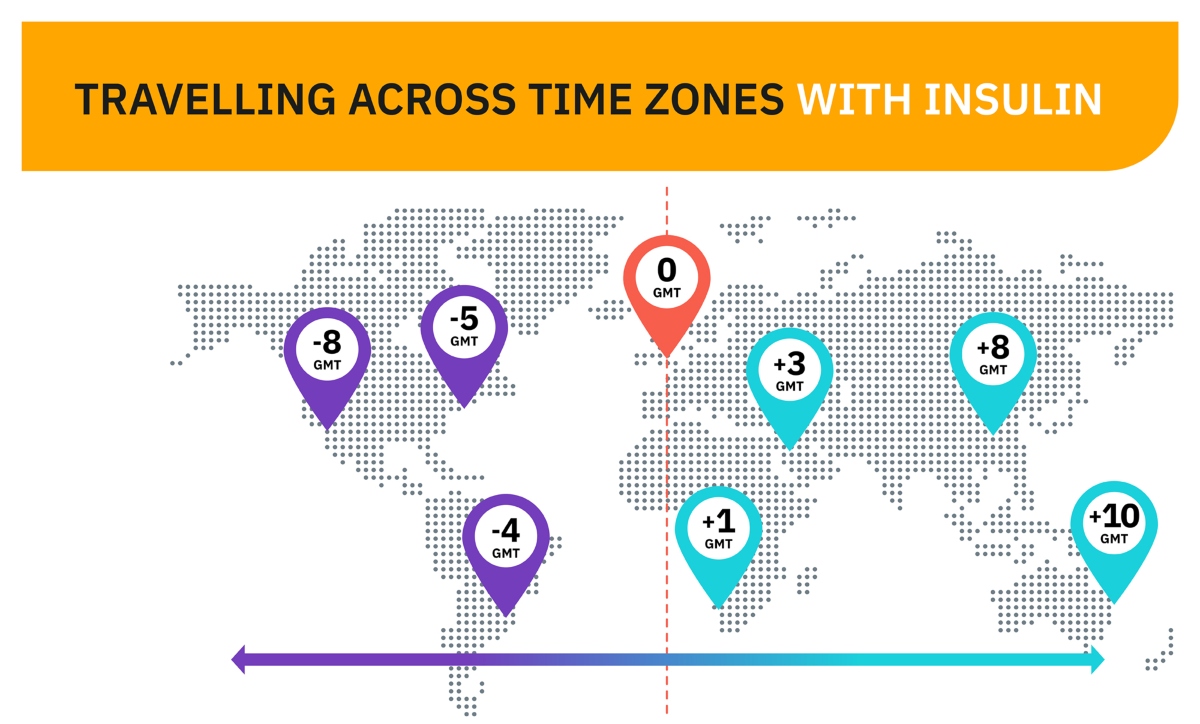
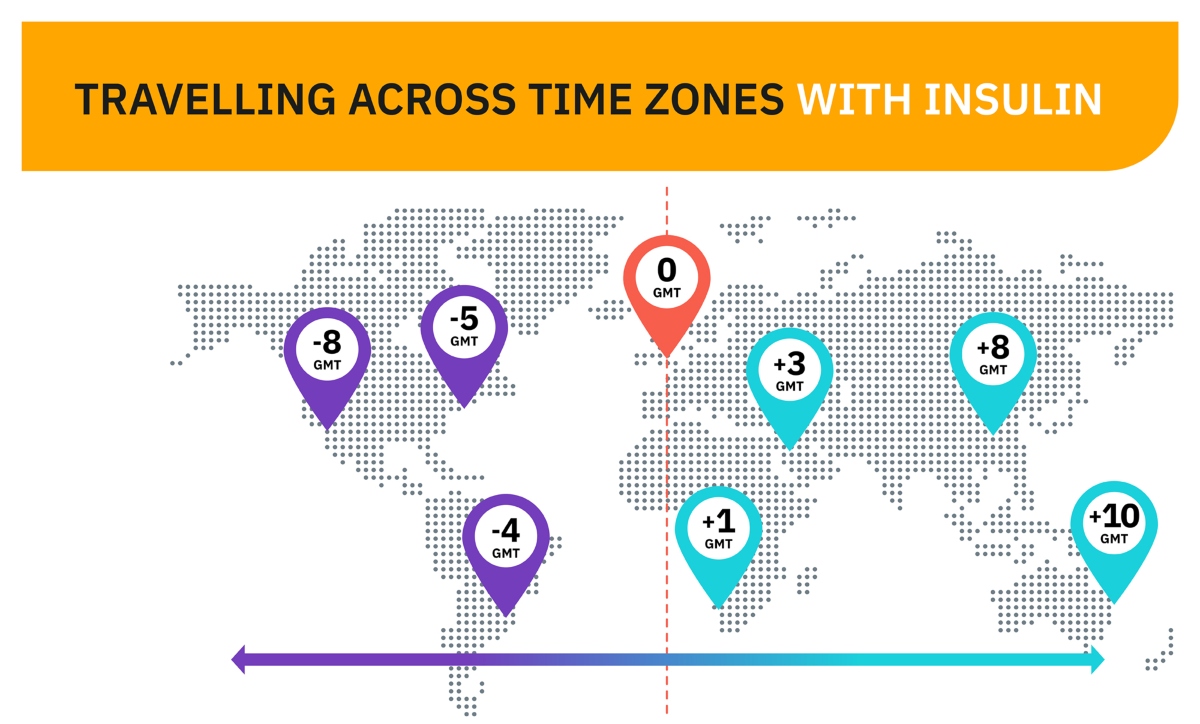
6. Changing time zones
Don’t forget to change the clock on your PDM/Controller to match your destination.
If you do not update your time zone, your insulin therapy will be delivered based on your old time zone, which may cause disruptions in your insulin delivery schedule and inaccurate history log.
You may need to adjust your Basal Programs on your PDM/Controller. (For Omnipod® 5, these are the programs you would typically follow in Manual Mode). For changes of just a few hours, basal rate adjustments are minor and easy to calculate.
For long-distance travel, however, figuring out the correct Basal Program can be more challenging. Your healthcare provider can help with these adjustments.
For Omnipod 5, the SmartBolus Calculator relies on accurate, updated insulin delivery history and data logging from your Omnipod 5 System. If a time zone change is detected by the Controller, the system will notify you.
Below is some information regarding travelling across specific time zones5, but you should speak to your healthcare provider about the best way to approach your diabetes management on your journey.
| INSULIN REGIMEN | TRAVELLING EAST TO WEST (LONGER DAY) | TRAVELLING WEST TO EAST (SHORTER DAY) |
| Once-daily long-acting insulin | Keep your watch at UK time while travelling and give it at your usual UK time. Once you arrive at your destination, move to your usual injection time (e.g. bedtime). | |
| You may need to give a smaller dose on the first day, as your previous dose may still be active. | ||
| Twice daily mixed insulin | Take your normal morning and evening doses while travelling, and then take half your evening dose with a meal when you arrive. | Take your normal morning and evening doses while travelling. |
| Long-acting insulin once or twice daily plus short-acting insulin with meals | Inject short-acting insulin with any meal that contains carbohydrate, no matter what time of day or night. If you take once-daily long-acting insulin, keep your watch at UK time and give it at your usual time until you arrive at your destination. | |
| Move to a convenient time, but if this is longer than 24 hours since your last injection, you may need to give a small dose of short-acting insulin to control blood glucose levels. | Move to a convenient time, but if this is shorter than 24 hours since your last injection, you may need to give a smaller dose of short-acting insulin with your last meal to avoid hypos. | |
| If you inject long-acting insulin twice a day, keep injection times roughly 12 hours apart while traveling. | ||
| Travel between different time zones becomes a lot easier. Wait until you arrive in the country you are visiting and then change the settings in your insulin pump to the local time. Consider switching your pump to flight mode during take-off, flight, and landing. | ||
7. Once you’ve arrived and managing type 1 diabetes while you are away
You may need to make some changes to your diabetes management in the first few days as you get used to a new routine, climate, activity level, and foods.
Jet lag may also impact your blood glucose levels, so keep monitoring them closely as your body adjusts to the new location.
Insulin may be absorbed more quickly in hot weather5, so keep extra glucose on hand to treat any hypos.
Food and alcohol will of course affect your blood sugar levels. Don’t be afraid to try different foods, just keep a supply of hypo treatments with you, and test your glucose levels regularly.
8. Accessing diabetes supplies at your destination
There are people living with type 1 diabetes all over the world, and healthcare services are available almost everywhere - a nearby pharmacy is a good starting point if you need more medical supplies.
As mentioned, you may want to look up the nearest pharmacies and medical centres before you leave. Take your copy of your prescription with you to help explain what it is that you need, as the brand names may be different in different countries6.
9. Keeping your insulin cool in hot climates
If you’re heading somewhere hot, medically approved cooling packs or wallets will help keep your insulin from spoiling in the heat.
Remember to keep all of your diabetes supplies out of direct sunlight as much as possible.
If you’re staying in a hotel, contact them ahead of your departure to check if there will be a fridge in your room to store your insulin. Some hotels may be able to supply one if you explain that it’s for medical reasons.
Remember to stay hydrated and protect yourself from the sun. But most of all, remember to have fun!
Share your experiences of travelling with Omnipod!
Do you have any inspiring travel stories with Omnipod? Have you overcome your travel fears for an amazing adventure? Has Omnipod helped you feel more confident about travel?
Share them with our Instagram community and show the world what’s possible with type 1 diabetes!
Simplify travelling with Omnipod
Omnipod is an insulin management system designed to Simplify Life® for people living with type 1 diabetes.
Each wearable, waterproof* Pod continuously delivers insulin for up to three days (72 hours) with no multiple daily injections and no insulin pump tubing.
Plus, with the Omnipod 5 Automated Insulin Delivery System you can enjoy the benefits of fewer lows, increased time in range and reduced HbA1c‡.
‡ When used in automatic mode with Dexcom G6 CGM, the Omnipod 5 System makes adjustments to insulin delivery every 5 minutes based on the user's current CGM value, glucose values predicted 60 minutes in the future, glucose trend, and past insulin delivery to bring glucose to a user defined target.
‡1.Study in 240 people with T1D aged 6 - 70 years involving 2 weeks standard diabetes therapy followed by 3 months Omnipod 5 use in Automated Mode. Average time with high blood glucose in adults/adolescents and children, standard therapy vs. 3-month Omnipod 5: 32.4% vs. 24.7%; 45.3% vs. 30.2%. Median time with low blood glucose in adults/adolescents and children, standard therapy vs. 3-mo Omnipod 5: 2.0% vs. 1.1%; 1.4% vs. 1.5%. Brown et al. Diabetes Care (2021).
‡ 2. Study in 80 people with T1D aged 2 - 5.9 yrs involving 2 weeks standard diabetes therapy followed by 3 months Omnipod 5 use in Automated Mode. Average time with high blood glucose (>180mg/dL) from CGM in standard therapy vs Omnipod 5 = 39.4% vs. 29.5%. Average time with low blood glucose (<70mg/dL) from CGM in standard therapy vs Omnipod 5 = 3.41% vs. 2.13%. Sherr JL, et al. Diabetes Care (2022).
Clinical study participants experienced a reduction in A1C of 0.71% in children aged 6-14 (0.55% in children aged 2-5.9 years of age) and 0.38% in adults.