Insulin Pumps Explained
What’s an insulin pump?
An insulin pump is a small, wearable device that can deliver insulin continuously throughout the day and night, often in very small doses. This can help with blood glucose control1.
Insulin pumps are an alternative way to deliver insulin for people with diabetes, in place of multiple daily injections (MDI).
Having different insulin delivery options means you can choose what suits your health and lifestyle needs best. This may change over time.
Although insulin pumps eliminate the need for injections, it is still recommended to carry back-up supplies in case of emergencies.
Different types of insulin pump
There is more than one type of insulin pump. What’s the difference?
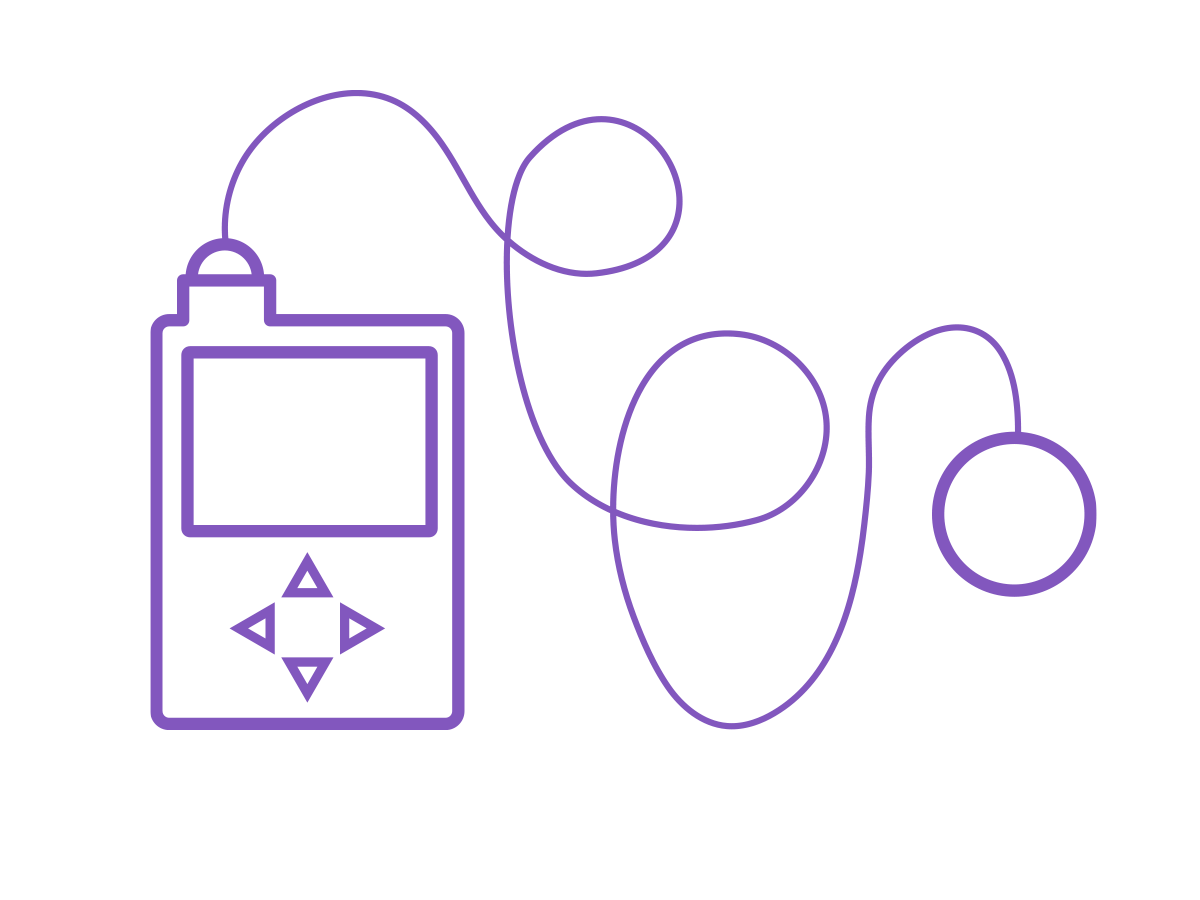
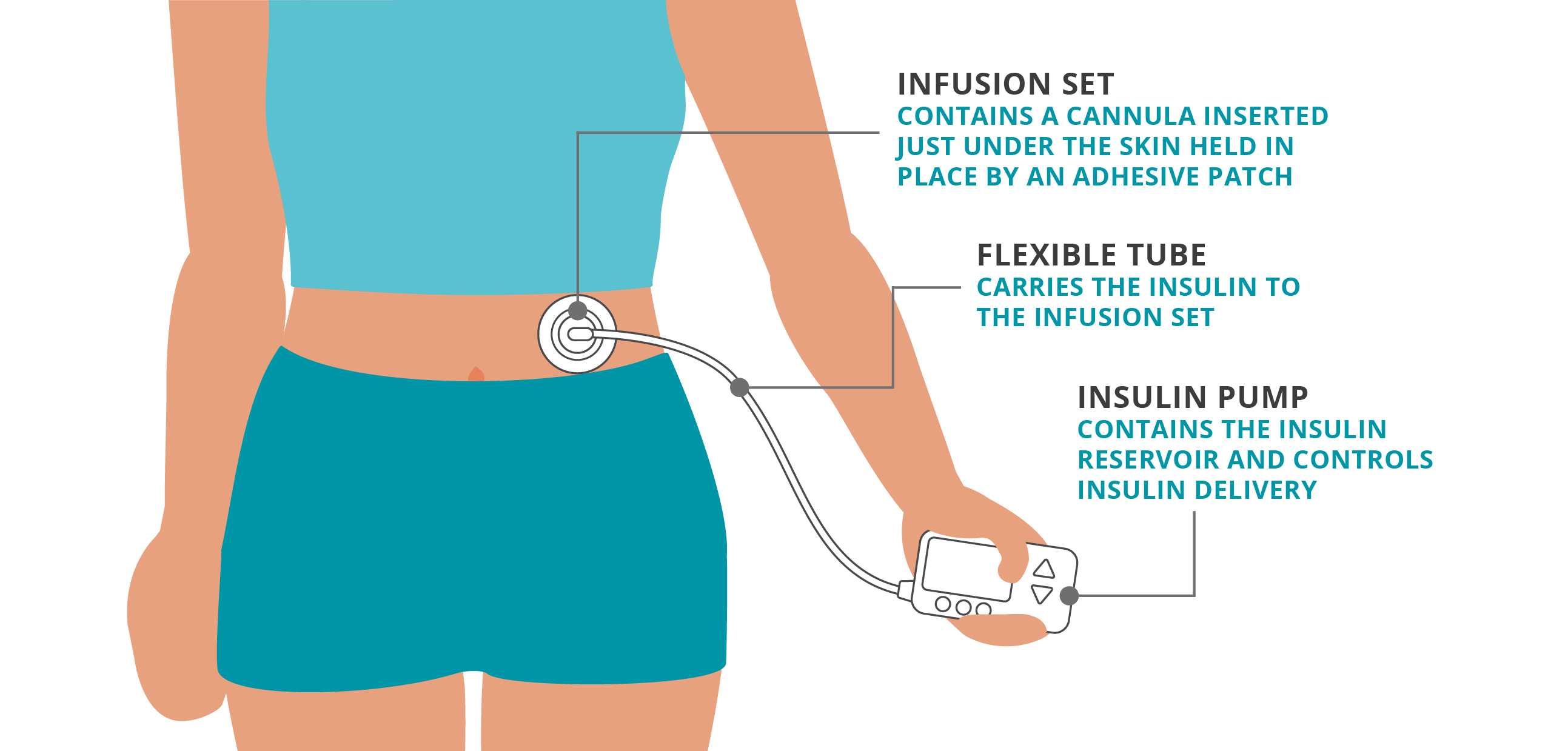
Tethered pumps
A traditional tethered or tubed pump contains the insulin in the pump itself. The insulin flows through a tube into the body through an infusion set. The pump is kept somewhere on the body, usually in a pocket, or clipped to a bra/belt.
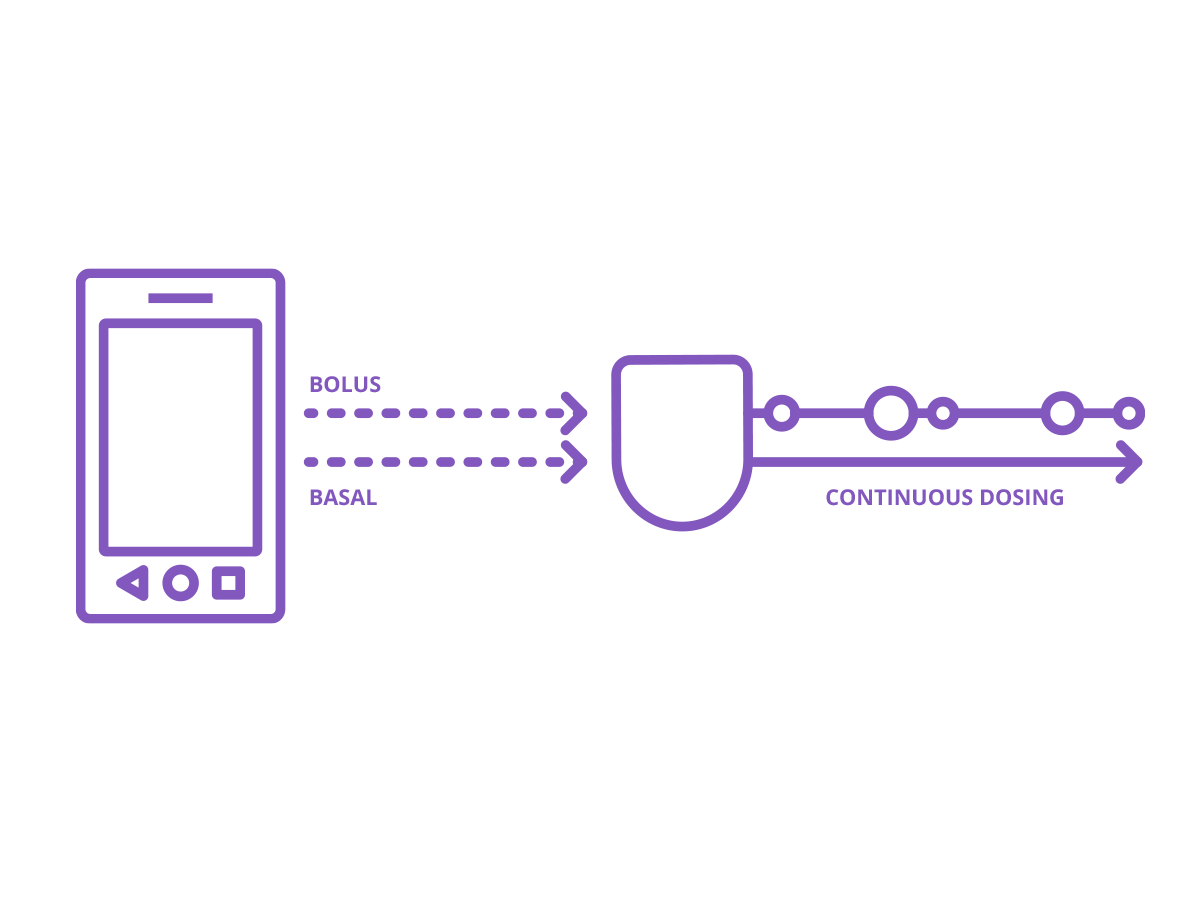
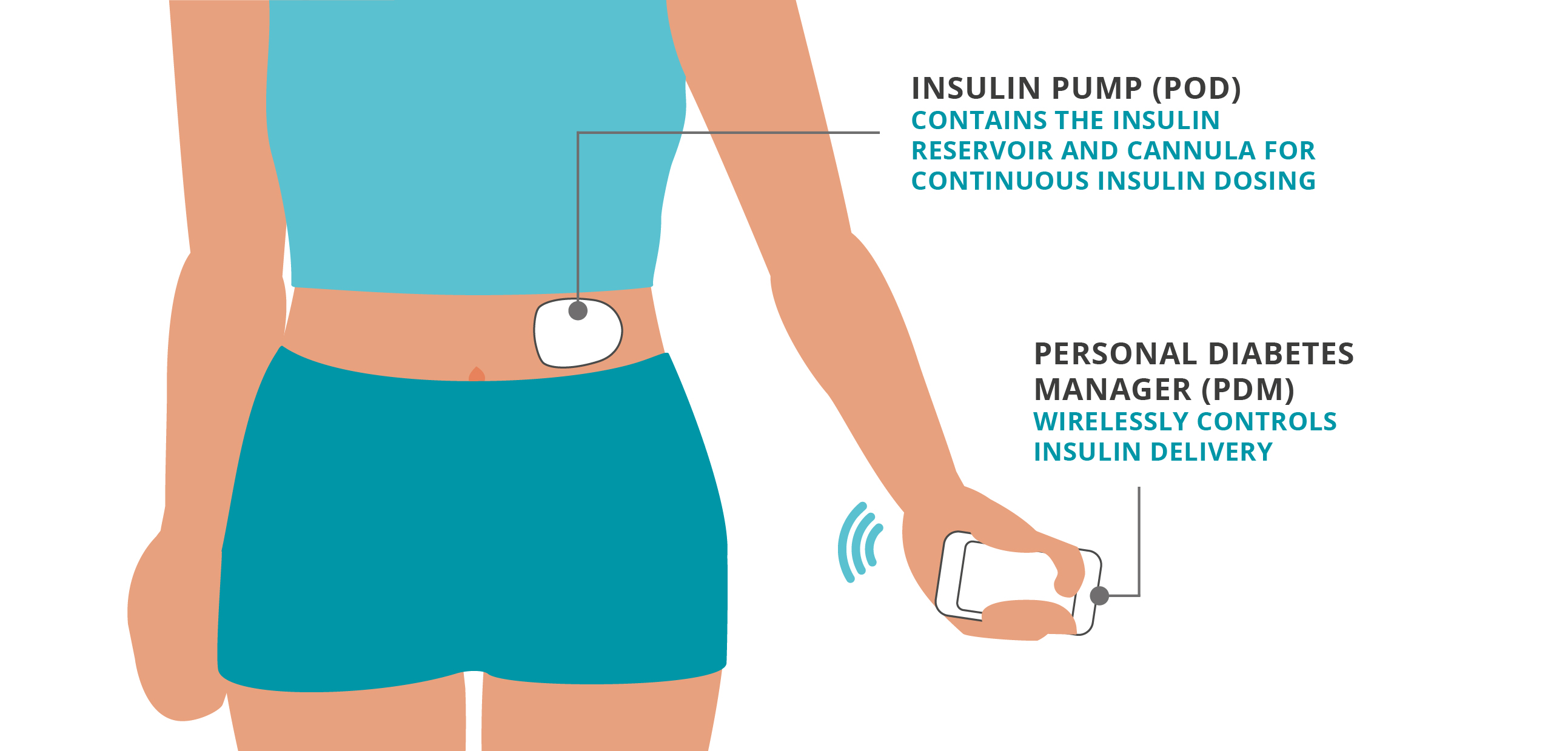
Patch pumps
A patch pump is sometimes called a tubeless or wireless pump. The part that contains the insulin sticks directly to the skin with adhesive, so there is no external connecting tube. Insulin is programmed from a separate device, like a remote or controller, which wirelessly communicates to the patch pump to deliver the insulin via a thin tube, called a cannula, inserted directly under the skin.
How does an insulin pump work?
A continuous amount of insulin is delivered 24 hours a day through a cannula placed under the skin. This is known as basal, or background insulin.
Additional insulin is delivered for meals and blood glucose corrections - these are known as bolus doses2.
Traditional pumps
Tubeless pumps
Insulin pumps can help you calculate your bolus doses. These will be based on a combination of your personal settings, glucose readings and the carbohydrate values for any food you’re eating.
You only need one type of insulin with an insulin pump, commonly known as fast-acting insulin. This is used for both your basal and bolus doses.
Don’t worry - if you or your child starts on an insulin pump, you will receive extensive training, either as an inpatient or outpatient3.
Understanding basal rates
Bolus insulin doses
Insulin pumps and glucose sensors
Insulin pump technology is moving - fast! This progress is positive for people with diabetes.
Some insulin pumps can integrate with certain glucose sensors (also known as continuous glucose monitors, or CGMs) to continuously adapt and automatically deliver basal insulin according to your personal needs.
This is what’s known as an Automated Insulin Delivery System (AID), which you may know as a Hybrid Closed Loop System (HCL).
We’ll look at this in more detail in a different module.


Other Frequently Asked Questions
Who qualifies for an insulin pump?
Are insulin pumps painful?
Can I shower with an insulin pump?
Do you sleep with an insulin pump?
Do I still need both types of insulin?
How much does it cost?
Next up...
References and Disclaimers:
2. Walsh, J, Roberts, R. Pumping Insulin. 6th ed. Torrey Pines Press. 2017.
3. https://www.diabinfo.de/en/living-with-diabetes/treatment/therapy-techniques.html
4. https://diabetesjournals.org/care/article/26/4/1079/23670/Insulin-Pump-TherapyA-meta-analysis
The information and other content provided in this article, or in any linked materials, are not intended and should not be construed as medical advice, nor is the information a substitute for professional medical expertise or treatment. If you or any other person has a medical question or concern, you should consult with your healthcare provider. Never disregard professional medical advice or delay in seeking it because of something that have read on this blog or in any linked materials. If you think you may have a medical emergency, call your doctor or emergency services immediately. The opinions and views expressed on this blog and website have no relation to those of any academic, hospital, health practice or other institution.